Neck/Shoulder/Arm Thoracic Outlet Syndrome
The thoracic outlet is a small space just behind and below your collarbone. The blood vessels and nerves that serve your arm and shoulder are located in this space.
There are 3 types of TOS. (nerve, vein, or artery).
Ninety-five percent (95%) of all cases of TOS are Neurogenic, which is compression of the nerves to the arm and shoulder. Venous TOS occurs only 3 to 4 percent of the time and is due to obstruction or clotting of the main vein to the arm, the subclavian vein. Arterial TOS, is the rarest type, occurring in only 1 percent of cases, and it is due to disease in the artery leading to the arm, the subclavian artery. Almost all cases of arterial TOS are associated with an extra rib (cervical rib) or an abnormal first rib.
Thoracic outlet syndrome (TOS) is the presence of a mixture of hand, arm, shoulder, and neck symptoms. All of these symptoms are due to pressure (or compression) against the nerves (called the brachial plexus) or blood vessels within the scalene triangle at the thoracic outlet.
The common symptoms depend on which structure is being compressed.
- Neurogenic TOS (nTOS), the symptoms are pain, numbness, tingling, and/or weakness in the arm and hand. Also common is a tired feeling in your arm, which is made worse by working with your arms raised over your head. Neck pain and headaches in the back of your head are also frequent symptoms. Another common occurrence is pain that starts in your shoulder and runs down your arm, as well as pain in your fingertips. One can even experience facial pain, jaw pain, ear pain and pain on the front of your chest. Unfortunately, the symptoms of neurogenic TOS can be vague and non-specific.
- Venous TOS (vTOS) is distinguished by swelling in your entire arm, plus pain and dark discoloration.
- Arterial TOS (aTOS) presents with pain, coldness, and a pale discoloration of the hand. Cramps occur when using the arm for activity.
Neurogenic TOS is most often the result of neck trauma such as a whiplash injury. Motor vehicle accidents, traction injuries to shoulder, slipping and falling on floors or ice, blunt injury to base of neck or top of shoulder, or repetitive stress from working on assembly lines are the common causes.
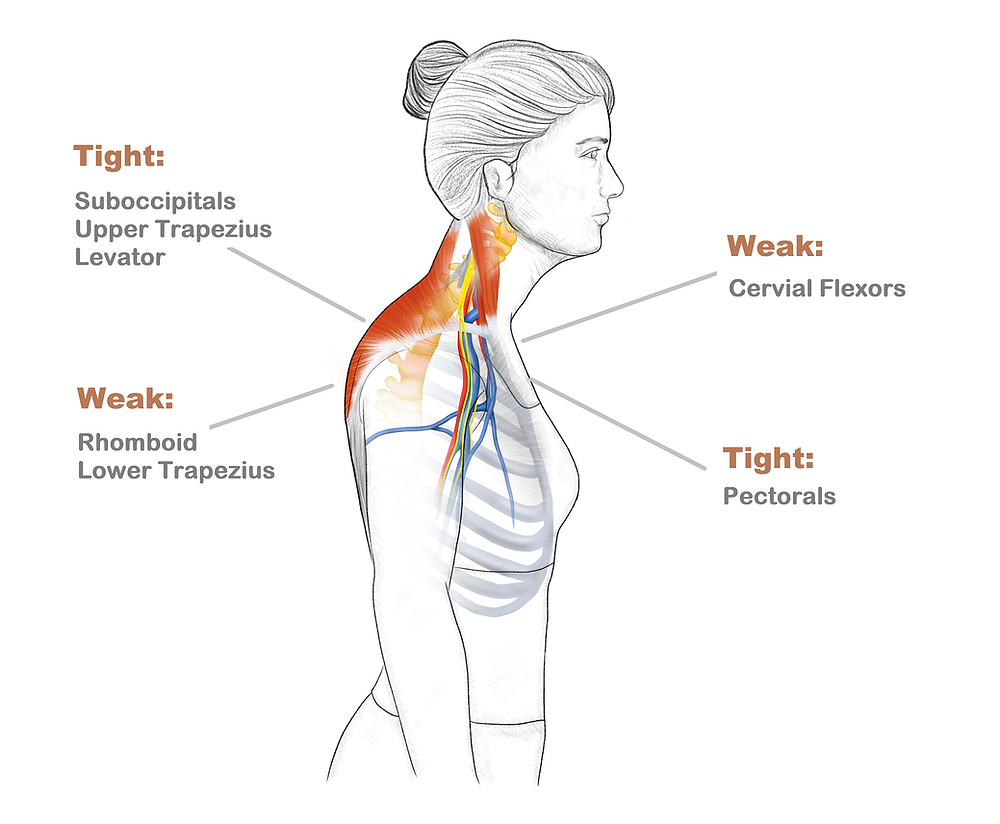
The symptoms are due to trauma and scar tissue formation in; neck muscles (called scalene muscles) and the nerves (brachial plexus). Congenital deformities of the first rib or having an anomalous cervical rib or band significantly increases the risk of acquiring this condition. Ultimately, the cause is compression and tethering of the brachial plexus nerves at the thoracic outlet.
Diagnosing TOS can be complex. It begins by your physician asking you a series of questions to find out your symptoms, the distribution of these symptoms and and how the symptoms began. Depending on your symptoms, the doctor will be able to tell if you might have a nerve, vein, or artery compression. An appropriate physical examination will be beneficial in determining your diagnosis as well. It is not uncommon that patients have seen several physicians and have been evaluated for cervical neck problems and shoulder problems prior to the referral for evaluation of thoracic outlet syndrome.
In arterial TOS, a physical exam often finds the pulse at your wrist is diminished or absent. Your hand may have a pale color compared to your pink, good hand.
Venous and arterial TOS are best diagnosed with the aid of specific tests, venography for venous TOS, and pulse volume or arteriography for arterial TOS.
Your treatment depends on the type of TOS you have, determined by your symptoms, exam, and test results.
Neurogenic TOS (nTOS): Initially treated with physical therapy, focusing on stretching, posture correction, and avoiding aggravating movements. Strengthening exercises may worsen symptoms. Therapy is followed by a home exercise program. Medications like muscle relaxants, NSAIDs, and steroids may help, along with heat or massage. If conservative treatments fail, ultrasound-guided injections or biologic therapeutics may provide relief. Surgery is considered if symptoms persist, involving the removal of certain neck muscles and scar tissue. First rib resection is rarely needed, as studies show no added benefit and higher complication risks. Surgery carries risks, and success rates vary (80–90% in specialized centers, 70% in general studies).
Venous TOS: Treated with clot-dissolving medication, blood thinners, or surgery to remove the clot. If necessary, the first rib may be removed to prevent recurrence, and angioplasty or vein repair may be performed.
Arterial TOS: Requires surgical repair or replacement of the damaged artery, often with a graft. The abnormal rib must be removed to prevent further damage, typically done in a single procedure.
- Surgical Approach to Injuries of the Cervical Plexus and Its Peripheral Nerve Branches. Brown DL, Dellon AL: Plast Reconstr Surg 141(4): 1021-1025, 2018. N/S/A/TOS
- Novel Surgical Approach for Decompression of the Scalene Triangle in Neuorgenic Thoracic Outlet Syndrome: Hagan R, Ricci J, Eberlin K, J Reconstr Microsurg 2018;34:315-320.
- Quadrangular space syndrome associated with superficial radial sensory neuropathy. Brown DL, Chung KC: Ann Plast Surg 43(2): 207-210, 1999. N/S/A/TOS
- Acute exertional compartment syndrome of the forearm. Dhawan V, Borschel GH, Brown DL: J Trauma 64(6): 1635-1637, 2008. Forearm/PMNC
Nerve Surgery Helps Relieve Chronic Pain
The majority of patients with chronic pain report significant decreases or complete resolution of their pain following nerve surgery. Most patients describe the ‘nerve pain feelings’ are improved as soon as the following day. Discomfort from the operation is frequently described as a completely different sensation, which subsides in the next few weeks.