Chronic Headache, Migraine, and Whiplash
Many people have headaches from time to time, but if you experience them on a daily or continual basis, your headaches may fall into the category of Chronic Migraine Headache.
At Neuropax, we have one of the most mature headache/migraine surgery practices in the nation or world. Our experience began in 2007 and has continued to mature, now greater than 15 years. We have continued to contribute to the field; advancing techniques, improving outcomes and teaching new surgeons. We have continued to lecture both nationally and internationally about our techniques, outcomes and research. We are committed to helping those suffering with chronic headache and migraine pain.
When traditional methods/medications have failed to resolve or control your headaches/migraines, you should be evaluated by a seasoned peripheral nerve surgeon with experience in headache surgery.
It is estimated that there are more than 40 million people are diagnosed with migraines in the United States. More than 6.5 million Americans are afflicted by chronic migraines, meaning they have migraine more than 15 days/month, many of these have co-existing, chronic daily headaches. We are still determining how many patients are suffering from forms of headaches that can be alleviated with surgery. We now know it is a much larger number than any of us expected. So many times, the headache type diagnosis, is a mis-diagnosis or even a missed-diagnosis.
Modern day best practices for treatment
At Neuropax, we have one of the most mature headache/migraine surgery practices in the nation or world. Our experience began in 2007 and has continued to mature, now greater than 15 years. We have continued to contribute to the field; advancing techniques, improving outcomes and teaching new surgeons. We have continued to lecture both nationally and internationally about our techniques, outcomes and research. We are committed to helping those suffering with chronic headache and migraine pain.
It is estimated that there are more than 40 million people are diagnosed with migraines in the United States. More than 6.5 million Americans are afflicted by chronic migraines, meaning they have migraine more than 15 days/month, many of these have co-existing, chronic daily headaches. We are still determining how many patients are suffering from forms of headaches that can be alleviated with surgery. We now know it is a much larger number than any of us expected. So many times, the headache type diagnosis, is a mis-diagnosis or even a missed-diagnosis.
When traditional methods/medications have failed to resolve or control your headaches/migraines, you should be evaluated by a seasoned peripheral nerve surgeon with experience in headache surgery.
Here at Neuropax we focus on determining whether there are any peripheral nerves in the head or neck areas that could account for chronic headache/migraine symptoms using a combination of a thorough history, a comprehensive physical exam and diagnostic nerve blocks. Determining if there is true migraine that is activated/triggered by the neuralgias or if there is only neuralgia is an important part of the evaluation.
Treating the neuralgia does cure head pain but does not cure migraine. However, importantly, it does relieve or treat an obnoxious trigger of the migraines. If we cure the neuralgia trigger you may still need to manage other triggers (i.e. stress, weather, gluten, etc.) If you do not have a history of migraine and your headaches started after trauma, surgery, or viral illness, there is a high likelihood that your headaches can be alleviated with surgery.
(Back of head / base of skull / upper neck)
- Occipital Neuralgia (ON)
- Occipital Nerve Syndrome (ONS)
- Nuchal Triangle Syndrome (NTS)
 The occipital region is the area in the back of the scalp/head. It is the most commonly surgically treated area for chronic headaches. When the headache pain occurs in the occipital region of the head and radiates to the forehead and behind the eyes, it is likely Occipital Neuralgia (ON). There are 3 different occipital nerves on each side of the head/neck. (Greater, Lessor and Third). Each of these nerves can be diagnosed with ON.
The occipital region is the area in the back of the scalp/head. It is the most commonly surgically treated area for chronic headaches. When the headache pain occurs in the occipital region of the head and radiates to the forehead and behind the eyes, it is likely Occipital Neuralgia (ON). There are 3 different occipital nerves on each side of the head/neck. (Greater, Lessor and Third). Each of these nerves can be diagnosed with ON.
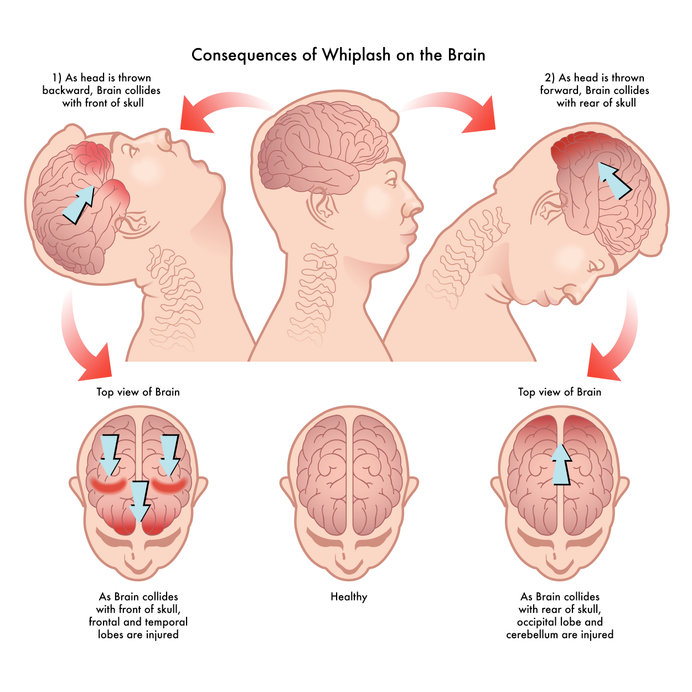
Occipital Nerve Syndrome (ONS) is the constellation of any or all the occipital nerves that have Occipital Neuralgia (ON). We have a long history of treating this condition and have developed stratified treatment pathways that individualize the patient’s unique clinical picture. We are integrated into the team of many providers at a much earlier point than historical pathways. The earlier we see you the better chance there is to successfully treat with more conservative options. This is particularly true with post-traumatic or post-whiplash headaches.
The diagnostic portion of the occipital nerve injection is what helps to confirm or validate the diagnosis of ON in each different nerve. Our novel techniques for therapeutic, ultrasound guided injections, if performed early enough, may obviate the need for surgery, particularly in the ONS patient population.
If surgery is recommended, then it is generally done through a single midline incision from the pointy protuberance in the back of your head down to the bottom of your hairline. It is done in an outpatient setting and you go home the same day. You will need 3 weeks for partial recovery and another 3 weeks to gradually return to all activities within reason. Success rates are now greater than 90%.
Nuchal Triangle Syndrome (NTS) is a subtype of Occipital Nerve Syndrome (ONS) that involves a more distal compression of the Greater (GON) and Lessor (LON) Occipital nerves and the Occipital artery. Inspired by Drs. Pietramaggori and Scherer original paper, we have named this sub-type of ONS as NTS. Identifying NTS commands an attentive practitioner to discriminate its patterns and subtle differences in the physical examination. Additionally, a different type of diagnostic block must be performed in order to confirm the diagnosis.
(** Neuralgia=“neur” (nerve) is causing the “algia” (pain). This is a general nerve term.)
(Front of head / forehead / behind the eyes)
- SupraOrbital Rim Syndrome (SORS)
 The frontal region is located, in the front of the head, specifically the forehead, brow and areas around the eyes. Supraorbital Rim Syndrome (SORS) is a constellation of the three nerves of the supraorbital rim. These include the supraorbital nerve (SON), supratrochlear nerve (STN), and zygomaticotemporal nerve (ZTN). These nerves can be compressed, neuralgic, or traumatized. The SON and the STN are compressed both at the boney orbital rim and at the myofascial sleeve of the corrugator muscle. Both of these compression sites on each nerve should always be addressed. We always preserve the SON, except for rare cases. The STN is often of small caliber if so is resected, if larger caliber it is preserved. The ZTN is a small caliber nerve and is routinely excised. Incision placement vary based on an individual, but all incisions are aesthetically designed to minimize any scar. You will having swelling the first week and then it diminishes. At the 3-week follow-up the swelling is essentially resolved. You can begin increasing activity at that time. Success rates are greater than 90%
The frontal region is located, in the front of the head, specifically the forehead, brow and areas around the eyes. Supraorbital Rim Syndrome (SORS) is a constellation of the three nerves of the supraorbital rim. These include the supraorbital nerve (SON), supratrochlear nerve (STN), and zygomaticotemporal nerve (ZTN). These nerves can be compressed, neuralgic, or traumatized. The SON and the STN are compressed both at the boney orbital rim and at the myofascial sleeve of the corrugator muscle. Both of these compression sites on each nerve should always be addressed. We always preserve the SON, except for rare cases. The STN is often of small caliber if so is resected, if larger caliber it is preserved. The ZTN is a small caliber nerve and is routinely excised. Incision placement vary based on an individual, but all incisions are aesthetically designed to minimize any scar. You will having swelling the first week and then it diminishes. At the 3-week follow-up the swelling is essentially resolved. You can begin increasing activity at that time. Success rates are greater than 90%
(Side of head / above ear / temple)
- Temporal Intersection Syndrome (TIS)
- Post-Traumatic Nummular Headache (PTNH)
The temporal region is located at the side of the head/scalp.
Temporal Intersection Syndrome (TIS).
 Temporal Intersection Syndrome (TIS). The main source of TIS is from the interaction of the Auriculotemporal Nerve (ATN) and Superficial Temporal Artery (STA). It can be of the anterior or vertical branches. The TIS may also involve the Zygomaticotemporal Nerve (ZTN) in many cases. The Lessor Occipital Nerve (LON) can also be a contributor to temporal headaches. TIS headaches are often described as icepick-like sharp stabbing pain that may or may not have a more diffuse pain. The pain may radiate towards the eye. Diagnostic blocks/injections are the primary test to help establish the diagnosis. In some cases, we will utilize therapeutic-type injections (steroid, Botox, etc.) when it meets certain our criteria. Surgical treatment is done in an outpatient setting. You go home the same day. There are minimal risks and return to normal life is short.
Temporal Intersection Syndrome (TIS). The main source of TIS is from the interaction of the Auriculotemporal Nerve (ATN) and Superficial Temporal Artery (STA). It can be of the anterior or vertical branches. The TIS may also involve the Zygomaticotemporal Nerve (ZTN) in many cases. The Lessor Occipital Nerve (LON) can also be a contributor to temporal headaches. TIS headaches are often described as icepick-like sharp stabbing pain that may or may not have a more diffuse pain. The pain may radiate towards the eye. Diagnostic blocks/injections are the primary test to help establish the diagnosis. In some cases, we will utilize therapeutic-type injections (steroid, Botox, etc.) when it meets certain our criteria. Surgical treatment is done in an outpatient setting. You go home the same day. There are minimal risks and return to normal life is short.
Post-Traumatic Nummular Headache (PTNH). Nummular essentially means circular. This describes the focal nature of these types of headaches. In our practice, the most common type of nummular headaches is after some form of trauma. They are typically located in areas where there is no muscle or very thin muscle over the bone in the head region. Most commonly they occur in the high temple or posterior temple region. It may have been where you hit your head during a fall, where you were hit in the head by an object, or even where you were hit during an assault. PTNHs are typically identified in the presence of other forms of headaches (SORS,TIS, or ONS)Diagnosis is established with a diagnostic nerve block / injection
If your headaches started after a traumatic injury or a surgery, you should definitely be evaluated to determine if neuralgias or nerve compressions are contributing to your overall headache burden.
If you have had chronic headaches or migraine and the numerous medicines have not resolved your pain or significantly diminished these headaches, you should be evaluated for nerve involvement as a major trigger or cause.
We at Neuropax Clinic were early adopters of this type of surgical treatment and now have one of the most mature experiences both nationally and internationally. We started developing our program in 2007 and have been a leading contributor to the evolution of techniques for these surgical procedures. We are considered a leading center of excellence and learning by our peers that perform this surgery.
There are now hundreds of peer reviewed publications supporting the benefit and outcomes of this headache and migraine surgery. Traditional headache providers, particularly the neurology community, have had a difficult time understanding the benefits of this treatment for certain headaches. We continue to collaborate with the non-surgical headache providers to help them understand which patients are best evaluated for this type of treatment. This is an effort to improve the overall stratified treatment pathways for patients with chronic migraine or acute post-traumatic headaches.
At Neuropax, we have a very thoughtful process to determine if surgery for your headaches/head pain/migraines is an option for you. We look at how they started, how long you have had them, the severity of your pain, the headache symptoms, the distribution and pattern of your headaches (frontal, temporal, occipital), a focused physical examination, and last, if you meet the criteria, a diagnostic nerve block will be performed. A positive response to the diagnostic injection/nerve block is the best prognostic indicator that we will be able to help in some way.
Nerve Decompression Surgery Can Reduce or End Your Migraine Headaches
The majority of patients with chronic pain report significant decreases or complete resolution of their pain. Most patients describe that the ‘nerve pain feelings’ are improved as soon as the following day. Discomfort from the operation is frequently described as a completely different sensation, which subsides in the next few weeks.