Foot Pain / Foot Drop
Common peroneal nerve injury at the knee can cause pain and loss of movement or sensation in the foot and leg.
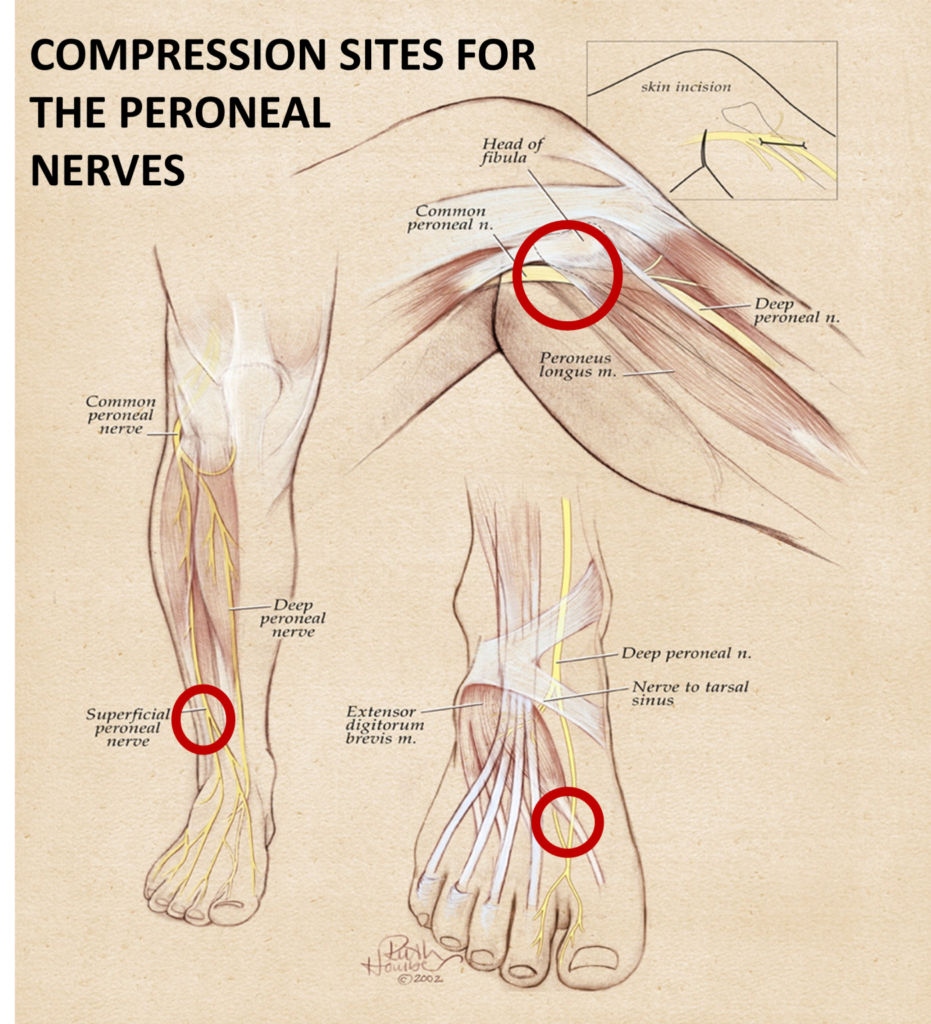
The peroneal nerve is a branch of the sciatic nerve, which supplies movement and sensation to the lower leg, foot and toes. Common peroneal nerve compression is a type of peripheral neuropathy (damage to nerves outside the brain or spinal cord). This condition can affect people of any age.
Injury of a single nerve, such as the common peroneal nerve, is called a mononeuropathy. Mononeuropathy means the nerve damage occurred in one area. However, certain body-wide conditions may also cause single nerve injuries.
Compression of a nerve injures the insulation cover around the nerve, and may destroy the nerve itself. There can be pain, numbness, weakness, and eventual loss of muscle mass because the nerves aren’t stimulating the muscles.
- Trauma or injury to the knee
- Fracture of the fibula (a bone of the lower leg)
- Use of a tight plaster cast (or other long-term constriction) of the lower leg
- Crossing the legs regularly
- Regularly wearing high boots
- Pressure to the knee from positions during deep sleep or coma
- Injury during knee surgery, from being placed in an awkward position during anesthesia, or from postoperative swelling.
- Who have had trauma or surgery to their leg
- Who are very thin
- With diabetic neuropathy
- With polyarteritis nodosa
- Who are exposed to certain toxins that can damage nerves
- Charcot-Marie-Tooth disease, an inherited disorder that affects all nerves.
- Decreased sensation, numbness, or tingling in the top of the foot or the outer part of the upper or lower leg
- Foot that drops (unable to hold the foot up at the ankle)
- “Slapping” gait (when each step makes a slapping noise)
- Toes drag while walking
- Walking problems
- Weakness of the ankles or feet
- Loss of muscle control in the lower legs and feet
- Atrophy of the foot or foreleg muscles
- Difficulty lifting up the foot and toes and making toe-out movements
Tests of nerve activity include:
- Electromyography (EMG, a test of electrical activity in muscles)
- Nerve conduction tests
- MRI
- Nerve ultrasound
Treatment aims to improve mobility and to decrease pain. Any illness or other cause of the neuropathy should be treated.
Surgical “release” or decompression is similar to carpal tunnel release. It is a straightforward outpatient operation that relieves the pressure on the nerve. Then, the nerve can repair itself.
You may need surgery if:
- The pain does not go away
- You have difficulty with walking or tripping (drop foot)
- There is evidence that the nerve is severely damaged
- Soleal Sling Syndrome (Proximal Tibial Nerve Compression): Results of Surgical Decompression; Williams E, Rosson G, Hagan R, Hashemi S, Dellon AL; Plastic and Reconstructive Surgery Journal, Volume 129(2).
- Denervation of the Periosteal Origin of the Adductor Muscles in Conjunction with Adductor Fasciotomy in the Surgical Treatment of Refractory Groin Pull; Dellon AL, Williams E, Rosson G, Hashemi S, Tollestrup T, Hagan R, Peled Z, Gurtmueller G, Ebmer J; Plastic and Reconstructive Surgery Journal, Volume 28(4).
- Tarsal Tunnel. Lyons DA, Brown DL: Neurosurgery by Example, Peripheral Nerve Volume, Selden ed; Yang and Wilson vol ed Oxford University Press, Ny, NY, 2017. Diab Neurop.
- Lower Extremity Contemporary Neuroma Management, Felder JM, Ko JH, Brown DL: Eberlein, Ed.; Springer, 2023. Knee Pain.
Nerve Surgery Helps Relieve Chronic Pain
The majority of patients with chronic pain report significant decreases or complete resolution of their pain following nerve surgery. Most patients describe the ‘nerve pain feelings’ are improved as soon as the following day. Discomfort from the operation is frequently described as a completely different sensation, which subsides in the next few weeks.