What Is Peripheral Nerve Pain?
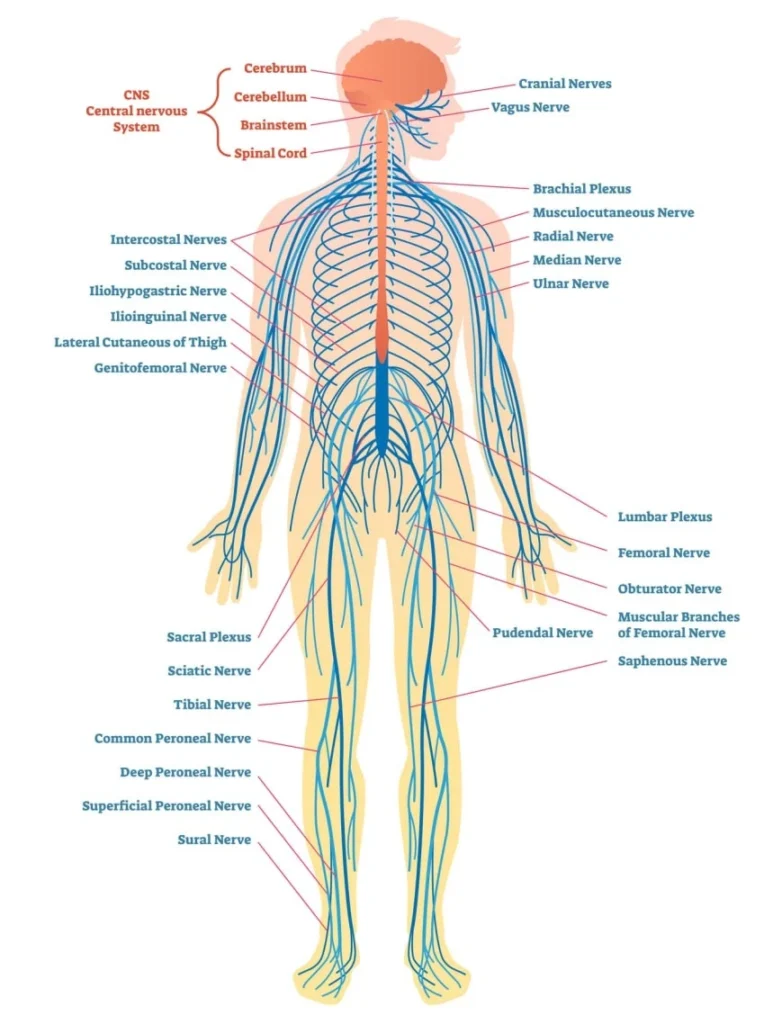
Peripheral nerves are all of the nerves outside of the brain and spinal cord: the nerves in your arms and legs, in your face, and in your chest, abdomen and back.
Whether caused by injury, surgery, or conditions such as diabetic neuropathy or shingles (post-herpetic neuropathy, PHN), damage to the peripheral nerves can lead to chronic pain that is difficult to diagnose and to find solutions to treat.
Our surgeons use cutting-edge treatments for pain caused by injury and/or compression of nerves.
New techniques are now available to reduce or eliminate pain for many patients. Neuropax Clinic is one of only a handful of institutions currently offering surgery as an option for patients who have exhausted other methods of treating their pain.
Many causes of chronic pain can be successfully treated with surgery. Chronic pain after operations, accidents, trauma, and sports injuries that has not been relieved by first-line methods may be due to injury to peripheral nerves. Patients often visit multiple doctors and engage in physical therapy, take medications, have orthopedic treatments or spinal nerve blocks without significant relief. Medications often only reduce or mask the symptoms — unfortunately, patients with chronic pain from peripheral nerve injury rarely experience lasting relief from medications.
The optimal patient for surgery has:
- Pain in a specific area for more than three months that has not been relieved by other methods like physical therapy or medications.
- A prior workup by other specialists such as orthopedic surgeons, physical medicine doctors, pain specialists, or neurologists — without discovering an obvious cause for the pain.
- Prior tests can be particularly helpful in suggesting nerve injury, such as MRIs, EMG/NCV, diagnostic nerve blocks, and MRIs.
You qualify for surgery if your pain has lasted more than 3 months following:
Prior Surgery
- Knee replacement (Knee Pain)
- Leg, ankle or foot operations (Foot Pain / Foot Drop)
- Hip replacement (Thigh Pain – Meralgia Paresthetica)
- Abdominal surgery, laparoscopic surgery, abdominoplasty, etc.
- Hernia repair (Groin / Hernia Pain)
- Mastectomy, breast reconstruction or augmentation (Post Mastectomy Pain Syndrome – PMPS)
- Chest surgery (Post Mastectomy Pain Syndrome – PMPS)
- Low Back pain with or without prior spine surgery
- Neck and facial surgery
- Amputations, including phantom pain (Amputation / Phantom Pain)
Trauma
- Falls (low back, buttock and leg pain)
- Sports injuries (ankle sprains, ligament tears)
- Car accidents, Whiplash
Compression
- Thoracic Outlet Syndrome (TOS)
- Carpal tunnel (Hand – Carpal Tunnel)
- Forearm (front and back) and Elbow Pain
- Abdominal Pain without another cause (ACNES)
- Nerve compression in the legs (lateral femoral, saphenous, peroneal nerves)
Other Causes
- Shingles – Post-herpetic Neuralgia (PHN)
- Diabetes
- New onset of foot pain, numbness or ulcers (Sole of the Foot Pain / Numbness – Tarsal Tunnel Syndrome)
Headaches
- Migraine Headaches
- Whiplash, Occipital Neuralgia
Diagnosing peripheral nerve injury as the cause for chronic pain is oftentimes quite straightforward. Surgeons at Neuropax Clinic can localize the cause and recommend treatment often within one visit. The process includes:
- A thorough patient history – when the pain started, potential causes, locations of pain, prior medical care
- A focused physical examination – to relate the pain to a particular nerve
- Nerve block – the doctor may suggest a local anesthetic numbing of the nerve(s) in order to confirm:
- That the pain is due to an injured nerve.
- Which nerve(s) are involved.
- Where is the injury to the nerve.
The type of procedure depends on the location and cause of the pain. In many instances, the pain results from compression of (pressure on) a specific nerve or group of nerves. In such cases, relieving the pressure relieves the pain. This can usually be accomplished through relatively small incisions during an outpatient operation. In other cases, the nerves may need to be divided and rerouted. This can result in a limited area of numbness of the skin — often a welcome trade-off for the pain!
Nerves do not like to be “squeezed’. There are some very narrow areas that nerves pass through – these areas are set-ups for compression of the nerve due to swelling or bruising from an injury, after surgery, or sometimes spontaneously. Examples of these types of compressions are carpal tunnel syndrome, common peroneal nerve, piriformis syndrome, lateral femoral cutaneous nerve, etc. If it is determined that your pain is due to compression of a nerve, an operation could be performed to relieve the pressure on the nerve. The tight space that the nerve goes through is opened surgically, giving it needed room to conduct signals normally, get good blood flow, and move normally.
Caused by Stretching, Cutting, Scar Tissue, etc.
Every operation has the potential to cause chronic nerve pain. By cutting through the tissues to correct another issue, small (often unseen nerves) can be cut or damaged. Retraction on tissues during surgery can stretch small nerves past their ‘breaking point’. After surgery, as tissues heal, nerves can be caught up in scar tissue, causing them to be pulled on every time the patient moves that area of the body. These injured nerves then send abnormal pain signals to the brain, causing chronic pain.
It is usually not possible to “fix” small nerves that are causing chronic pain, back to their original state of function. However, once the injured nerve is identified, surgeons can disconnect the nerves up-stream from the injury. This significantly decreases, or even eliminates, the chronic pain. An area of numbness is the trade-off, in place of the pain. Most patients are happy to make this trade!
Nerve resection has high success rates in treating nerve injury pain – around 80%, depending on the individual patient. In order to increase the chances for success even further, special treatments have recently been developed to “cap” the end of the cut nerves. Grafts of nearby muscle or skin are often placed around the ends of the nerve during surgery to prevent them from regrowing and causing pain again. These procedures, developed and pioneered at the University of Michigan, are called Regenerative Peripheral Nerve Interface (RPNI – muscle grafts) and Dermatosensory Peripheral Nerve Interface (DSPNI – skin grafts). The grafts are usually taken from nearby tissues, without additional harm to the patient. The goal is to give the new ends of the nerves something to grow into, thereby preventing the recurrence of nerve pain. These techniques have been used to treat nerve pain and phantom pain due to amputations, surgery and injury all over the body.
- Reset Neurectomy for Cutaneous Nerve Injuries. Hagan R, Eberlin K, Pickrell B, Hamaguchi R. PRS Global Open Journal. 2021 Feb, 15th. Doi: 10.1097 HNPTS
- State-of-the-Art Techniques in Treating Peripheral Nerve Injury. Kubiak CA, Kung TA, Brown DL, Cederna PS, Kemp SWP: Plast Reconstr Surg 141(3): 702-710, 2018. HNPTS
- Current State of the Surgical Treatment of Terminal Neuromas. Ives GC, Kung TA, Nghiem BT, Ursu DC, Brown DL, Cederna PS, Kemp SWP: Neurosurgery 83(3): 354-364, 2018. HNPTS
- Principles of nerve repair and reconstruction and neuroma management. Kubiak CA, Brown DL: Grabb and Smith’s Plastic Surgery, Chung, Wolters Kluwer, 2019. 8th, 10, 87-96. HNPTS
- Dermatosensory Peripheral Nerve Interfaces: Prevention of Pain Recurrence Following Sensory Neurectomy. Hart SE, Brown DL: Hand Clin 37(3): 383-389, 2021. HNPTS
- Unmasked Neuropathic Pain After Neurectomy: A Case Series and Review of the Literature. Gomez-Rexrode AE, Kennedy SH, Brown DL: Plast Reconstr Surg Glob Open.11(8): e5221, 08/2023. HNPTS & FAQ: MPMTALAS
- Management of Neuropathic Pain with Neurectomy Combined with Dermal Sensory Regenerative Peripheral Nerve Interface (DS-RPNI). Hespe GE, Brown DL: Semin Plas Surg. HNPTS
Nerve Surgery Helps Relieve Chronic Pain
The majority of patients with chronic pain report significant decreases or complete resolution of their pain following nerve surgery. Most patients describe the ‘nerve pain feelings’ are improved as soon as the following day. Discomfort from the operation is frequently described as a completely different sensation, which subsides in the next few weeks.