Post Mastectomy Pain "PMPS"
and Pain after Chest Surgery
Chronic Pain After Mastectomy and Chest Surgery
Reports indicate that 40 to 60 percent of patients who undergo mastectomy suffer from chronic pain — pain lasting longer than three years. Studies have demonstrated that patients with post-mastectomy pain experience a significantly worse quality of life with respect to physical well-being, physical autonomy, relationships, and psychological well-being. Long-term pain leads to decreased work function, increased healthcare utilization, and increased depression risk. Even breast biopsy, lumpectomy, breast augmentation and breast reconstruction can result in chronic breast and chest pain.
Our experience shows that post-mastectomy pain can be similar to pain experienced by limb amputation patients, with average pain scores of 8 out of 10! Therefore, post-mastectomy pain has far-reaching physical and psychological consequences. Patients with chronic post-mastectomy pain can also experience significant discomfort from even minor irritations like the touch of bedsheets or clothing, seat belts, coughing, or even giving a hug.
Peripheral neve surgery may be an option for patients experiencing chronic post-mastectomy pain.
Visit the PERIPHERAL NERVE PAIN PAGE or contact Neuropax Clinic at 314-434-7784 to learn more about this option.
Nerve Injury Contributes to Post-Mastectomy Pain
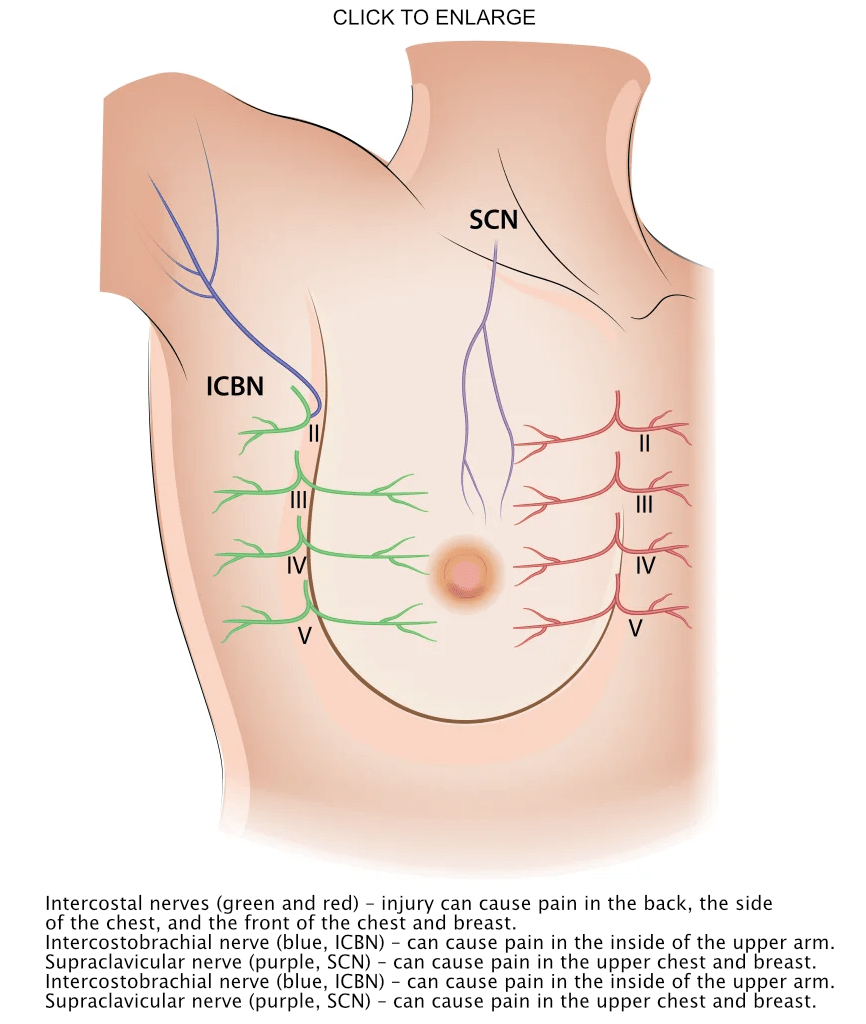
Studies have demonstrated that sensory nerve injury provides a substantial contribution to post-mastectomy pain. This is not surprising, given that multiple small sensory nerves are injured during breast surgery including mastectomy: the intercostal sensory nerves, the intercostobrachial nerve, and the supraclavicular nerve.
When breast tissue is surgically removed from the chest, sensory nerves traveling through these tissues are transected, stretched, or caught up in scar during the healing process. These nerve injuries can lead to chronic pain due to the development of what are known as end neuromas, neuromas-in-continuity, and scar compression. We have proven that the chronic pain is coming from these injured nerve(s).
Medication Treatments for Nerve Pain Are Often Not Enough
Opioids, NSAIDs such as ibuprofen, and neuropathic drugs including gabapentin or amitriptyline are sometimes helpful in managing the pain to acceptable levels. However, these treatments are often insufficient due to incomplete pain relief, inconsistent administration, and adverse effects including chronic dependence (opioids), gastrointestinal distress (NSAIDs), and dizziness and fatigue (neuropathic drugs).
Post-Mastectomy Pain and Opioid Dependence
In a very large study of insurance data, over 10% of patients who had not previously taken narcotic pain medications continued to use them for more than 3 months after breast surgery. These patients often require opioid doses that approximate those doses taken by chronic opioid users. These are very concerning statistics which highlight a significant problem!
Nerve Pain Can Be Easily Identified in the Clinic Setting
Our experience shows that injured nerves can be readily identified as the source of pain. During your visit, the surgeon will listen to your description of your pain, and perform an examination designed to pinpoint the location of pain-causing, injured nerves. You may be offered the opportunity to have a small injection of local anesthetic that may relieve the pain for a few hours by blocking the signals from the nerve(s). If successful, you will be able to experience the numbness, which comes as a trade-off for the pain. In cases where the feeling from the local numbing injection is preferable, your surgeon may discuss the potential for surgery to create this situation permanently.
Intercostal Nerves Causing Chronic Pain Can Be Safely Removed
Once nerve injury is identified as the source for the pain, surgical removal of the small, offending nerves can be performed in a straightforward outpatient operation. Small incisions on the flank (directly under the armpit) or just to the side of the breastbone or the spine are used to gain access to small nerves that come out to the skin from between the ribs. The damaged nerves are excised, with the anticipation of permanent resolution of the pain. The side effect is numbness in the area. Most patients accept this numbness as a welcome trade-off.
Nerve Surgery Helps Relieve Chronic Pain Following Breast Surgery
The majority of patients with chronic pain report significant decreases or complete resolution of their pain. It is uncommon, but there is the possibility of no improvement, or increase in the pain. Most patients describe that the ‘nerve pain feelings’ are improved as soon as the following day. Discomfort from the operation is frequently described as a completely different sensation, which subsides in the next few weeks.